THE BIRTH OF
A DIVISION
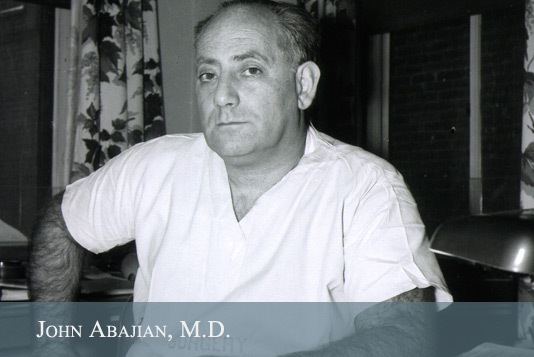
After Ford left,
John Abajian came
to Burlington with
a directive to create
a department for
anesthesiology at Mary Fletcher Hospital. A city boy who
attended Long Island University and New
York Medical College, Kreutz notes that
Abajian arrived in Vermont feeling like he
had been “banished to Siberia.” He quickly
earned a reputation as both brilliant
and difficult.
Almost immediately, some members of the
UVM medical staff were put off by Abajian’s
personality: cocky, opinionated, and extremely
outspoken, he made enemies easily. It turned
out that he was a very good anesthesiologist,
though, and he “managed to survive the next
few months.” Soon “known and admired by
the surgeons for his great intellect, innovative
ideas, and capable performance of his duties,”
Abajian later credited some of them — Al
Mackay, Walford “Wally” Rees, Keith Truax,
Lyman Allen, even old George Sabin — with
helping him through his turbulent first year in
Burlington. He also singled out T.S. Brown, who
became “like a second father” to him, saying:
“The only thing I really regret now is that I
wasn’t born a Vermonter. The type of cooperation
I received from people at the Fletcher at that
time, and from the medical school, is the best
any anesthesiologist could obtain and receive
anywhere in the United States.”
Abajian soon
recruited 24
year-old nurse
anesthetist
Elizabeth “Betty”
Wells to his
newfound division.
The techniques
they used where “atypical for the era,” Kreutz notes, with
a focus on local and regional anesthesia.
Although it’s unclear why he preferred these
methods, the duo continued to shape the
practice of anesthesiology through their
partnership. Wells later proved to be
indispensable, as World War II began to
call men into military service.
JOHN ABA JIAN GOES TO WAR
 Abajian enlisted in the U.S. Army in 1942,
and headed off to war. He eventually became
consulting anesthesiologist to General
George Patton, traveling throughout the
European Theater teaching nurses and
physicians in the field “fundamental
anesthesia techniques, pre-and postoperative
care, and shock and transfusion therapy.”
Kreutz says Abajian focused on regional
and local anesthesia as opposed to general,
just as he had done in Vermont. His work
is credited with saving many soldiers’ lives.
Abajian enlisted in the U.S. Army in 1942,
and headed off to war. He eventually became
consulting anesthesiologist to General
George Patton, traveling throughout the
European Theater teaching nurses and
physicians in the field “fundamental
anesthesia techniques, pre-and postoperative
care, and shock and transfusion therapy.”
Kreutz says Abajian focused on regional
and local anesthesia as opposed to general,
just as he had done in Vermont. His work
is credited with saving many soldiers’ lives.
George Patton’s Army was the epitome of a
hard charging, hard hitting, mobile warfare
unit, but it endured tremendous losses in
the process — from August 1944 through
April 1945, it suffered over 91,000 battle
casualties. During that period its overall
mortality rate fell significantly, though, from
2.9 percent in mid-1944 to 2.6 percent in
1945, and it’s possible that John Abajian’s
work at field and evacuation hospitals was one
of the reasons for the improvement. Patton
may have thought so, for he recommended
Abajian for the Legion of Merit. Odom also
credited Abajian for his “most useful” work,
writing in a postwar summary:
“By the time Major Abajian left a unit, he
had succeeded in giving valuable instruction in both the theory and practice of the
administration of anesthetics and had also
given valuable assistance in the handling of
casualties in the operating room. His work
elevated the standards of both anesthesia
and surgery in the Third U.S. Army.”
Abajian returned to the United States in
June of 1945 at the rank of Lieutenant
Colonel, and resumed his position at
UVM at the start of 1946.
THE HOME
FRONT
With Abajian
traversing Europe
with Patton’s
Army, back in
Vermont, Wells
became the leader
of the new division
at 25 years-old, caring for patients with
tireless dedication. She was joined by another nurse, Esther “Jackie” Roberts,
whom Kreutz describes as a “plain-spoken
farm girl from Barnard, Vt.,” and internist
Christopher Terrien Sr., a 1936 grad of the
UVM College of Medicine. The young
team handled the situation with remarkable
grace, according to Kreutz’s reporting.
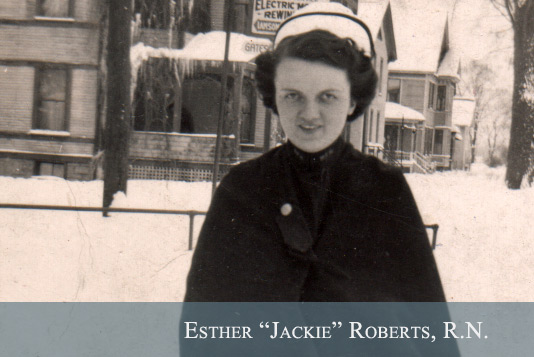
Despite the workload and risks, Wells later
wrote, “We survived the frequent call schedule
and, more importantly, our patients did too.
There were no fatalities due to anesthesia
during that period — I probably would have
resigned if there had been.” But by 1944, Wells
and Roberts were worn out and asked Mary
Fletcher Hospital’s new Superintendent, Lester
Richwagen, for more help. He obliged, hiring
Mary Fletcher School of Nursing graduates
Frances Wool in May 1944 and Florence
“Peg” Thompson in January 1945.
As World War II wound down, and
anticipating the return of many young men
seeking employment, the nurse anesthetists
who had put in countless long days and
call hours caring for patients during the war
explored their career options.
Kreutz notes that Wells and Thompson
continued to work in anesthesiology,
while Wool joined the military before
serving as a private nurse in New
Hampshire. Roberts found success in a
different medical field — she went on
to serve as surgical assistant to eminent
UVM neurosurgeon R.M.P. Donaghy,
who pioneered microsurgery, and in
1969, she was honored as the “Mother of
Microneurosurgery.” She died in South
Burlington, Vt., in 2010, at the age of 90.
BUILDING A DIVISION
With men returning from the war eager
for additional training and employment,
a postwar directive from the American
Medical Association urged “hospitals
around the country to expand their postwar
residency programs.” With a Division
of Anesthesiology once again under the
leadership of Abajian, UVM did just that,
setting up a residency program and hiring
its first anesthesia resident, Antonio Bayuk,
in July of 1946. A veteran who had been
injured in a parachute jump in Germany, he
was soon joined by a second resident, Ernie
Mills, also a veteran. Additional residents
followed, including Donald Harwood and
Charles Cox. These early residents recall
both the challenges and the rewards of
working in a rapidly changing field.
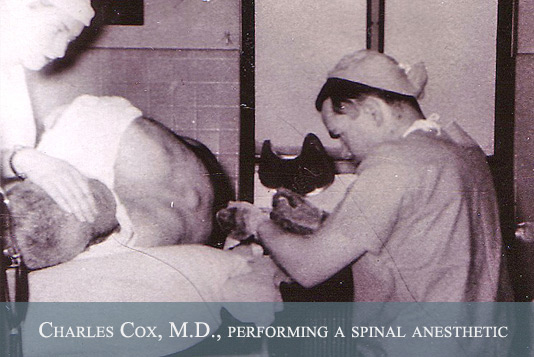
Anesthesia was still a relatively dangerous
business in the early 1950s, with primitive
agents (ether and cyclopropane) and
crude monitoring (primarily a “finger on the
pulse”), but the residents learned to deal
with it. “Safety was primordial,” according to
Francesca deGerman. “This is why we used
local, blocks, spinals, continuous spinals, and
general anesthesia, in that order.” Harwood
remembered that he “learned to be suspicious
of redheads and fast-pulsed patients.” Cox
noted that he didn’t lose a single patient during
his residency, a remarkable achievement.
Betty Wells and Ernie Mills did most of the
teaching that took place. “Betty and Ernie and
dear experience were our mentors,” Harwood
recalled:
“I learned that we would be integrated
into the thick of things very rapidly and it was
sink or swim…. John gave us an unfettered
opportunity to get into trouble on our own and
get back out of it if we could…. [He] helped
us cultivate intuition.”
These first residents helped to lay the
foundation for a robust division that
would go on to make some important
discoveries in the field.