/com-top-tier-images/deansnewsletter/recurring_graphics/dean_newsletterheader_600px_blue(2).jpg?sfvrsn=3b747039_2)
July 14, 2021 | Volume III, Issue 13
Weaving Social Medicine Through the Vermont Integrated Curriculum
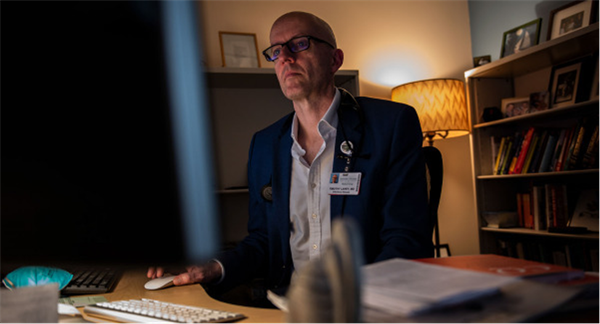
Undoing historical injustices hinges, in part, on open, honest discussion about the historical and cultural roots of injustice, says Timothy Lahey, M.D, M.M.Sc., professor of medicine and director of clinical ethics at UVM Medical Center. Giving medical students the opportunity to have those conversations early and often fosters an awareness that stands to help change the system.
“Understanding the social determinants of health and the incentives and history that inform them can help us identify real tools for change,” he says. “That can convert a will to fairness into a concrete plan that in fact yields it.”Dr. Lahey seeks to foster open discussion about the social determinants of health and other ethics topics through 16 ethics session woven throughout the first-year Foundations of Clinical Science course. These sessions complement multiple other ways medical students can learn about social justice at Larner, from the student-run Social Medicine Theme of the Week to social justice-related sessions throughout the pre-clinical curriculum.
The weekly ethics sessions consist of pre-reading and a quiz, followed by in-class discussion. Dr. Lahey frequently links the sessions to current events, encouraging students to apply their understanding of medical ethics to an ever-changing world. For instance, during the height of the COVID-19 pandemic in the United States, Lahey added a session on resilience.
“I wanted the students to see how resilience relates intimately to ethics,” he says. “If people are feeling under-fire, under-appreciated, and sleep-deprived, we know that they are much more likely to do something unethical.”
(This article is excerpted from a story that will appear in the next issue of Vermont Medicine.)
Pictured above: Dr. Lahey working in his office.

2021 Faculty Promotions and Reappoitments
One of the most important milestones of an academic career is a promotion in rank. This year, several Larner College of Medicine faculty members hit that milestone, being put forward by their chairs and Dean Richard Page, M.D., and approved for reappointment or promotion by Provost and Senior Vice President Patty Prelock, Ph.D.
“The promotion in rank denotes evaluation by one’s peers and the assessment of one’s contributions to the college’s missions by recognizing excellence in research, service and teaching,” says Charles Irvin, Ph.D.,associate
dean for faculty affairs. “I encourage the Larner community to join me in congratulating all those who were promoted this year in honor of their accomplishments.”
Faculty who received promotions or reappointments this year are:
Thomas Ahern, Ph.D., M.P.H. - Promotion to Associate Professor of Surgery with tenure; Dmitriy Akselrod, M.D. - Promotion to Associate Professor of Radiology, Clinical Scholar Pathway; Erik Anderson, M.D. -
Promotion to Associate Professor of Anesthesiology, Clinical Scholar Pathway; Michael Blankstein, M.D. - Promotion to Associate Professor of Orthopaedics and Rehabilitation, Clinical Scholar Pathway; Jason Botten, Ph.D. -
Promotion to Professor of Medicine (Tenure); Christopher Brady, M.D., M.H.S. - Promotion to Associate Professor of Surgery, Clinical Scholar Pathway; Martin Chang, M.D., Ph.D. - Promotion to Professor
of Pathology and Laboratory Medicine, Clinical Scholar Pathway; Mark Charlson, M.D. - Promotion to Associate Professor of Orthopaedics and Rehabilitation, Clinical Scholar Pathway; Allison Ciolino, M.D. -
Promotion to Associate Professor of Pathology and Laboratory Medicine, Clinical Scholar Pathway; Keith Curtis, M.D. - Promotion to Associate Professor of Surgery, Clinical Scholar Pathway; Thomas Delaney, Ph.D. -
Promotion to Associate Professor of Pediatrics, Education Scholar Pathway; Katherine Devitt, M.D. - Promotion to Associate Professor of Pathology and Laboratory Medicine, Clinical Scholar Pathway; Julie Dragon, Ph.D. -
Promotion to Associate Professor of Microbiology and Molecular Genetics, Research Scholar Pathway; Julie Dumas, Ph.D. - Associate Professor of Psychiatry, awarded tenure; Navid Esfandiari, Ph.D. -
Promotion to Professor of Obstetrics, Gynecology and Reproductive Sciences, Clinical Scholar Pathway; Nathalie Feldman, M.D. - Promotion to Associate Professor of Obstetrics, Gynecology and Reproductive Sciences, Education
Scholar Pathway; Jonathan Flyer, M.D. - Promotion to Associate Professor of Pediatrics, Clinical Scholar Pathway; Andrew Goodwin, M.D. - Promotion to Professor of Pathology and Laboratory Medicine,
Clinical Scholar Pathway; Rebecca Guy, Ph.D. - Promotion to Assistant Professor of Microbiology and Molecular Genetics, Education Scholar Pathway; Jessica Heath, M.D. - Promotion to Associate Professor
of Pediatrics, Clinical Scholar Pathway; Chris Holmes, M.D., Ph.D. - Promotion to Professor of Medicine (Tenure); Peter Holoch, M.D. - Promotion to Associate Professor of Surgery, Clinical Scholar
Pathway; C. Matthew Kinsey, M.D., M.P.H. - Promotion to Associate Professor of Medicine with tenure; David Lunardini, M.D. - Promotion to Associate Professor of Orthopaedics and Rehabilitation,
Clinical Scholar Pathway; Stephen Merena, D.P.M. - Promotion to Associate Professor of Orthopaedics and Rehabilitation, Clinical Scholar Pathway; Anne Morris, M.D. - Promotion to Associate Professor
of Family Medicine, Clinical Scholar Pathway; Nathaniel Nelms, M.D. - Promotion to Associate Professor of Orthopaedics and Rehabilitation, Clinical Scholar Pathway; Michael Previs, Ph.D. -
Second Reappointment as Assistant Professor of Molecular Physiology & Biophysics, Tenure Pathway; Delphine Quenet, Ph.D. - Second Reappointment as Assistant Professor of Biochemistry, Tenure Pathway; Tamara Rimash, M.D. -
Promotion to Associate Professor of Surgery, Clinical Scholar Pathway; Andrew Rosenfeld, M.D. - Promotion to Associate Professor of Psychiatry, Clinical Scholar Pathway; Sarah Schlein, M.D. - Promotion
to Associate Professor of Surgery, Clinical Scholar Pathway; David Seward, M.D., Ph.D. - Second Reappointment as Assistant Professor of Pathology and Laboratory Medicine, Tenure Pathway; Stacey Sigmon, Ph.D. -
Promotion to Professor of Psychiatry (Tenure); Emily Stebbins, M.D. - Promotion to Associate Professor of Anesthesiology, Clinical Scholar Pathway; Alissa Thomas, M.D. - Promotion to Associate
Professor of Neurological Sciences, Clinical Scholar Pathway; Adrianus (Jos) Van der Velden, Ph.D. - Promotion to Associate Professor of Pathology and Laboratory Medicine, Research Scholar Pathway; Rebecca Wilcox, M.D. -
Promotion to Professor of Pathology and Laboratory Medicine, Clinical Scholar Pathway; Leslie Young, M.D. - Promotion to Associate Professor of Pediatrics, Clinical Scholar Pathway; Neil Zakai, M.D. M.Sc. -
Promotion to Professor of Medicine (Tenure)
Image above: Light green, dark green, and yellow graphic with text that reads “Faculty Promotions."

UVM & Partners’ RAPID Trial Supports Treatment to Reduce Death in Moderately Sick COVID-19 Patients
Results from an international grassroots-funded multicenter clinical trial co-led by Professor of Medicine Mary Cushman, M.D., M.Sc., show that giving a full dose of heparin early to moderately ill hospitalized COVID-19
patients could reduce the risk of severe disease and death.
The RAPID Trial was designed to detect differences in the primary outcomes of moderately ill hospitalized COVID-19 patients, such as ICU admission, mechanical ventilation, or death. Participants were randomized to receive either a therapeutic full dose
or prophylactic low dose of heparin – a blood thinner given regularly at low dose to hospitalized patients to stop clots from forming and reduce inflammation.
Support for the trial came from Defence Research Development Canada, St. Michael’s Hospital Foundation, St. Joseph’s Healthcare Foundation, participating institutional grants—including a UVM Medical Center Fund Grant and support from
the Vermont Center for Cardiovascular and Brain Health COBRE—and even a GoFundMe campaign, among other sources.
Co-PIs with Dr. Cushman are Michelle Sholzberg, M.D.C.M., M.Sc., and Peter Jüni, M.D., of St. Michael’s Hospital of Unity Health Toronto and the University of Toronto.
Read the full article about the study.

New Scholarship/Loan Forgiveness Program Targets Vermonters' Health Care Needs
The inaugural offering of the VT AHEC Scholars Medical Student Incentive Scholarship/Loan Forgiveness Program has been announced for Larner third-year (Class of 2023) and fourth-year (Class of 2022) medical students who are pursuing primary care, including family medicine, internal medicine, pediatrics, obstetrics-gynecology, or psychiatry, and who are committed to future practice in rural Vermont. Up to ten awards that are anticipated to be $40,000 each will be made in this initial round.
This program was established by the Vermont legislature in collaboration with the Vermont Department of Health, the UVM Larner College of Medicine’s Office of Primary Care and AHEC Program, and the Vermont Student Assistance Corporation (VSAC) to strengthen the primary care workforce pipeline and increase the number of new physicians practicing in Vermont to meet the health care needs of Vermonters, with a focus on rural areas and undersupplied medical specialties.
The Office of Primary Care and AHEC Program will host an information session, including opportunities for Q & A, on Wednesday, July 21 at 12:00 p.m. to 1:00 p.m. via Zoom at: https://uvmcom.zoom.us/j/96367835176.
Learn more about this new scholarship/loan forgiveness program.
Pictured above: Charles Maclean, M.D. (far left), associate dean for primary care and professor of medicine, examines a patient while a medical student observes.

With June and all its rainbow fanfare just behind us, it's essential to remember that healthcare, and in particular LGBTQ+ healthcare, is inherently political. As we are writing this piece, a record number of anti-transgender laws have been enacted across the country, with more bills introduced and awaiting approval in various state legislatures...Disparities in access and treatment of transgender people do not end with Pride Month. Even though the rainbow flags will be put away and corporations will move on to their next PR campaign, transgender individuals will continue to be discriminated against and denied access to healthcare......As future physicians, what can we do?”
– Bradley Blansky & Rachel Adelsheim, Class of 2023 medical students.
Read Bradley Blanksy and Rachel Adelsheim Larner College of Medicine blog post, “Beyond the Rainbow Flag: Improving Health Care for Transgender Individuals.”
Recommend a staff member to highlight in Larner Medicine!
Accolades & Appointments



The Department of Surgery recognized the following faculty members recently:
- Robert Raut, M.D., assistant professor of surgery in the Division of Ophthalmology, received the “H. Gordon Page Clinician Award” for the Dedication and Commitment to Excellence in Patient Care;
- Krista Evans, M.D., assistant professor of surgery in the Division of General Surgery, received the “John H. Davis Service Award” for Unselfish Service and Dedication to the Goals and Visions of the Department;
- Richard Bounds, M.D., associate professor of surgery in the Division of Emergency Medicine, received the “Jerome S. Abrams Teaching Award” for Dedication and Commitment in Excellence in Education;
- Roz King, MSN, RN, CNL, research program manager in the Division of Emergency Medicine in the Department of Surgery, received the “James E. Demeules Research Award” for the Dedication and Commitment to Excellence in Research.
The Teaching Academy has announced the names and levels of its newest and advancing members as of Spring 2021. They are as follows:
- Bridget Marroquin, M.D., Associate Professor of Anesthesiology
- Jesse Moore, M.D., Associate Professor of Surgery
Master Teacher
- Kevin Abnet, M.D., Associate Professor of Anesthesiology
- John Klick, M.D., Associate Professor of Anesthesiology
- Thomas Lahiri, M.D., Professor of Pediatrics
- Emily Stebbins, M.D., Assistant Professor of Anesthesiology
Member
- Lee-Anna Burgess, M.D., Assistant Professor of Medicine
- Joanna Conant, M.D., Assistant Professor of Pathology and Laboratory Medicine
- Rebecca Evans, M.D., Assistant Professor of Anesthesiology
- Abigail Hielscher, Ph.D., Assistant Professor of Neurological Sciences
- K. Elliott Higgins, M.D., Assistant Professor of Anesthesiology
- Breena Holmes, M.D., Associate Professor of Pediatrics
- Sherrie Khadanga, M.D., Assistant Professor of Medicine
- John Miller, M.D., Assistant Professor of Medicine
- Delphine Quénet, Ph.D., Assistant Professor of Biochemistry
- Elly Riser, M.D., Assistant Professor of Medicine.
CITATION HIGHLIGHTS
Long B, Willis GC, Lentz S, Koyfman A, Gottlieb M. Diagnosis and Management of the Critically Ill Adult Patient with Hyperglycemic Hyperosmolar State. J Emerg Med. 2021 Jul 10:S0736-4679(21)00465-0. doi: 10.1016/j.jemermed.2021.05.008. Epub ahead of print. PMID: 34256953.
Oliver AC, DeSarno M, Irvin CG, Kaminsky D, Tidey JW, Sigmon SC, Heil SH, Gaalema DE, Lee D, Bunn JY, Davis DR, Streck JM, Gallagher T, Higgins ST. Effects of Reduced Nicotine Content Cigarettes on Fractional Exhaled Nitric Oxide (FeNO) and Self-Reported Respiratory Health Outcomes among Smokers with Psychiatric Conditions or Socioeconomic Disadvantage. Nicotine Tob Res. 2021 Jul 13:ntab145. doi: 10.1093/ntr/ntab145. Epub ahead of print. PMID: 34255068.
Nourbakhsh B, Waubant E, Evers AWM, Solomon AJ. Ethical considerations in the treatment of multiple sclerosis fatigue. Mult Scler Relat Disord. 2021 Jul 3;54:103129. doi: 10.1016/j.msard.2021.103129. Epub ahead of print. PMID: 34247106.
Long B, Liang SY, Lentz S. High flow nasal cannula for adult acute hypoxemic respiratory failure in the ED setting: A narrative review. Am J Emerg Med. 2021 Jul 3;49:352-359. doi: 10.1016/j.ajem.2021.06.074. Epub ahead of print. PMID: 34246166.
Otto AK, Soriano EC, Birmingham WC, Vadaparampil ST, Heyman RE, Ellington L, Reblin M. Impact of Relationship and Communication Variables on Ambulatory Blood Pressure in Advanced Cancer Caregivers.Ann Behav Med. 2021 Jul 9:kaab057. doi: 10.1093/abm/kaab057. Epub ahead of print. PMID: 34244701.
Hale T, Angrist N, Hale AJ, Kira B, Majumdar S, Petherick A, Phillips T, Sridhar D, Thompson RN, Webster S, Zhang Y. Government responses and COVID-19 deaths: Global evidence across multiple pandemic waves.PLoS One. 2021 Jul 9;16(7):e0253116. doi: 10.1371/journal.pone.0253116. PMID: 34242239.
Shabani M, Bakhshi H, Ostovaneh MR, Ma X, Wu CO, Ambale-Venkatesh B, Blaha MJ, Allison MA, Budoff MJ, Cushman M, Tracy RP, Herrington DM, Szklo M, Cox C, Bluemke DA, Lima JAC. Temporal change in inflammatory biomarkers and risk of cardiovascular events: the Multi-ethnic Study of Atherosclerosis. ESC Heart Fail. 2021 Jul 9. doi: 10.1002/ehf2.13445. Epub ahead of print. PMID: 34240828.
Ricotta DN, Hale AJ, Freed JA, Scribner TE, Zeidel ML, Herzig SJ. Generalists as Clinical Physiologists: Bringing Science Back to the Bedside. J Gen Intern Med. 2021 Jul 8. doi: 10.1007/s11606-021-06978-0. Epub ahead of print. PMID: 34240283.
Crothers JW, Chu ND, Nguyen LTT, Phillips M, Collins C, Fortner K, Del Rio- Guerra R, Lavoie B, Callas P, Velez M, Cohn A, Elliott RJ, Wong WF, Vo E, Wilcox R, Smith M, Kassam Z, Budd R, Alm EJ, Mawe GM, Moses PL. Daily, oral FMT for long-term maintenance therapy in ulcerative colitis: results of a single-center, prospective, randomized pilot study. BMC Gastroenterol. 2021 Jul 8;21(1):281. doi: 10.1186/s12876-021-01856-9. PMID: 34238227; PMCID: PMC8268596.
Barnum MS, Boyd ED, Vacek P, Slauterbeck JR, Beynnon BD. Association of Geometric Characteristics of Knee Anatomy (Alpha Angle and Intercondylar Notch Type) With Noncontact ACL Injury. Am J Sports Med. 2021 Jul 8:3635465211023750. doi: 10.1177/03635465211023750. Epub ahead of print. PMID: 34236929.
GRANTS REPORT: UVM SPONSORED PROGRAM ADMINISTRATION
Annual/Monthly Reports for Sponsored Projects
WHAT'S HAPPENING
LCOM Events Calendar | UVM Events Calendar | LCOM Student Activities Calendar
Feedback? Contact Us!
View Archive | Subscribe
Published by the Office of Medical Communications
The Larner College of Medicine
at The University of Vermont
Copyright 2021



